Narrow Angle Glaucoma Facts
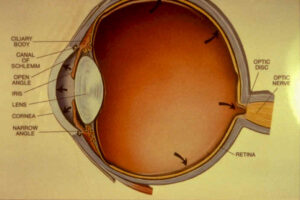
Photo Credit: curtmerrick via Flickr CC2.0
A narrow angle glaucoma diagnosis can be scary. Although it can be very serious, narrow angle glaucoma can also be quite manageable with proper identification and treatment.
What Is Narrow Angle Glaucoma?
Narrow angle glaucoma (also known as acute angle glaucoma or closed-angle glaucoma) is an eye condition that occurs when fluid builds up behind the iris. The buildup of fluid can cause a sudden and dangerous increase in the pressure behind the eye, known as ‘intraocular pressure’. This pressure can cause serious damage to the infected eyes over time.
Narrow Angle Glaucoma vs Open Angle Glaucoma
It can be helpful to understand the difference between the two primary types of glaucoma to better understand what is causing the issue and how to approach treatment.
Open angle glaucoma occurs when the drainage canal of the eye is not completely blocked, but only partially blocked. Think of open angle glaucoma like a clogged drain. Eye fluid drainage is significantly reduced, which is what causes the buildup of fluid over time. Open angle glaucoma is painless and can easily fly under the radar if you do not get regular eye exams.
With narrow angle glaucoma, the drainage canal of the eye is very narrow, which is the cause of the reduced drainage and fluid buildup. This particular type of glaucoma is more common in far sighted individuals. Narrow angle glaucoma is more dangerous than open angle glaucoma because the drainage canal can easily become completely blocked, resulting in a very rapid buildup of pressure that can cause severe permanent damage if not immediately addressed.
Rest assured that millions of Americans live long and healthy lives with glaucoma. However, early identification and treatment are essential to preventing long-term, irreversible damage to the eye.
Narrow Angle Glaucoma Symptoms
Many patients are asymptomatic, meaning there are no noticeable symptoms upon diagnosis, which makes regular check-ups even more important. However, some patients do experience dramatic and sudden symptoms.
Knowing what symptoms to look for is key to proper identification:
- Hazy or blurred vision
- Severe eye or head pain
- Cloudy cornea
- Upset stomach or vomiting (with eye pain)
- Appearance of rainbow-colored circles or halos around lights
- Dilated pupils
- Red eyes
- Sudden vision loss
If you feel that you have any of the above symptoms, please seek medical assistance immediately.
Causes Of Narrow Angle Glaucoma
There are several factors that can cause narrow angle glaucoma:
- Defect in eye structure
- Eye trauma
- Pupillary block
- Iris plateau
- Hyperopia
- Tumors
- Severe diabetic eye disease
Regular checkups with your eye doctor can help identify these conditions.
Risk Factors For Narrow Angle Glaucoma
Although narrow angle glaucoma does not discriminate, certain demographics are at a higher risk for this condition:
- Farsightedness – Farsighted individuals are more likely to develop narrow angle glaucoma
- Age – Aging can cause changes to the anatomy of the eye, increasing the risk of glaucoma
- Race – Asians and Eskimos are at a slightly higher risk of developing narrow angle glaucoma because they typically have a more shallow anterior eye chamber and anatomically narrow angles
- Sex – Women are at a slightly higher risk of developing narrow angle glaucoma
- Cataracts – Cataracts can cause changes to the eye that can cause pupillary blockage, which can lead to the development of narrow angle glaucoma
Narrow Angle Glaucoma Diagnosis
Regular checkups are essential to proper eye health and condition diagnosis. This is especially true because narrow angle (and other types of) glaucoma can be completely asymptomatic. Both men and women should begin to receive a glaucoma evaluation at the age of 35 and then again at the age of 40. Individuals who are at a higher risk of developing glaucoma (as noted above) and individuals over the age of 60 should have their eyes checked annually.
Glaucoma diagnosis is achieved through eye pressure measurement. Your eye doctor will perform a ‘tonometry check’ that is gently pressed against the eye to measure and record the pressure.
Additionally, an ophthalmoscope is used to examine the precise shape and color of the optic nerve by magnifying a light into the center of the eye. If the optic nerve appears abnormal or damaged, additional tests may be run.
A gonioscope is used to measure the angle where the iris meets the cornea and to determine if the angle is open or closed. This measurement determines the specific type of glaucoma for diagnosis and treatment.
Additional tests might include a perimetry test, which produces a complete map or your field of vision, and a pachymetry test, which measures the thickness of the cornea.
Early detection through regular eye exams is key to long-term vision health.
Narrow Angle Glaucoma Impacts
One of the primary impacts of narrow angle glaucoma occurs with the rapid increase in intraocular pressure, which can damage the optic nerve that transmits images from the eye to the brain. The buildup of pressure can also deteriorate the peripheral vision over time. Long-term vision loss is possible, but proper diagnosis and treatment often prevents this potential side effect. Though there is no cure for glaucoma, and an aggressive treatment plan can help prevent long-term damage and vision loss.
Narrow Angle Glaucoma Treatment
Upon diagnosis, treatment for narrow angle glaucoma will start immediately. Topical eye drops are administered to lower the pressure of the eye as quickly as possible. Additionally, an oral medication called ‘acetazolamide’ may be given to also reduce the pressure and eye fluid systems simultaneously. Some physicians may administer a drink solution like isosorbide or mannitol in some cases to lower the pressure.
If the condition persists, your eye doctor may perform a laser-based procedure called ‘peripheral iridotomy’, which entails making a very small hole in the iris that allows fluid to escape. The procedure is relatively painless and only takes 10 minutes.
Filtration surgery is a final, more invasive option for treatment when medication and drainage efforts fail to control eye pressure long-term. The procedure creates a completely new drainage channel to allow eye fluid to properly drain.

